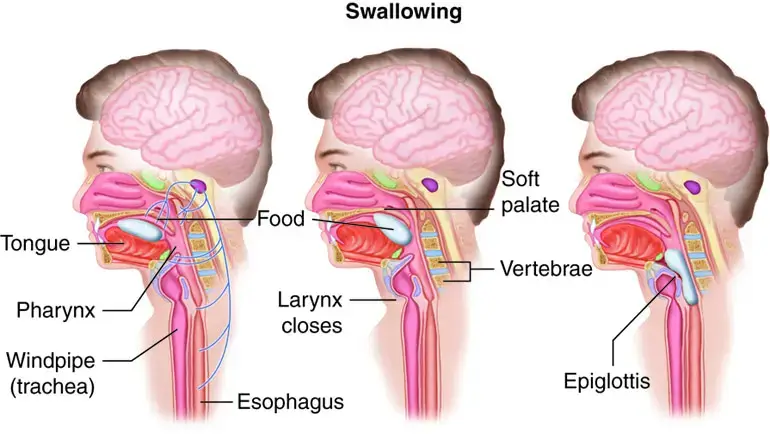
Dysphagia, or difficulty swallowing, is a condition that can range from mild to severe, affecting individuals differently. It is crucial to quantify the severity of dysphagia to develop an appropriate treatment plan and track the progression or improvement of the condition over time.
While the World Health Organization (WHO) does not provide a specific grading system for dysphagia, several other widely accepted scales are used to assess and grade dysphagia. The choice of scale often depends on the specific context, the patient’s condition, and the healthcare setting.
The Dysphagia Outcome and Severity Scale (DOSS)
The DOSS is a seven-level scale used to systematically rate the severity of dysphagia based on observations of the patient’s eating and drinking[^1^]. It ranges from level 1 (severe dysphagia, non-oral feeding recommended) to level 7 (normal, oral feeding with no restrictions).
Overview of the DOSS
The DOSS was developed to provide clinicians with a standardized method to categorize the severity of a patient’s dysphagia, ensuring consistent assessment and documentation across different clinical settings. The scale takes into account the patient’s safety and efficiency of swallowing, helping professionals determine appropriate interventions and diet recommendations.
Breakdown of the DOSS Levels
- Level 1 (Severe Dysphagia): Individuals at this level are typically non-oral feeders. The risk of aspiration is high, and they often rely on alternative methods of nutrition, such as feeding tubes.
- Level 2: Patients can consume a limited oral diet but rely primarily on non-oral feeding methods. Aspiration risk remains high.
- Level 3: Individuals can manage a limited diet with consistent textures, but there’s still a significant risk of aspiration.
- Level 4: Patients are generally restricted to a single texture of food, like pureed or thickened liquids, to minimize the risk of aspiration.
- Level 5: Individuals can manage a variety of textures but with specific limitations, often excluding the most challenging foods or liquids.
- Level 6: Patients can consume most foods and liquids safely but may need to employ compensatory strategies or avoid specific challenging items.
- Level 7 (Normal): Individuals at this level have a normal swallowing function and can eat or drink without restrictions.
The Functional Oral Intake Scale (FOIS)
The FOIS is another seven-level scale, but it focuses on the types of food or liquid the individual can consume and their dependence on tube or intravenous feeding[^2^].
Absolutely! The Functional Oral Intake Scale (FOIS) is a pivotal tool for understanding and categorizing an individual’s ability to consume various food and liquid textures. It is a patient-centric scale, focusing on the practical aspects of day-to-day oral intake. Here’s a more in-depth look:
Understanding Dysphagia and Oral Intake
Dysphagia, or difficulty swallowing, can significantly impact an individual’s ability to consume foods and liquids safely. This can have far-reaching consequences, including malnutrition, dehydration, and aspiration pneumonia. While various scales and tools are used to assess the nature and severity of dysphagia, the FOIS provides a more functional perspective, focusing on the individual’s daily consumption abilities.
Overview of the FOIS
The FOIS is a clinician-reported scale, which means that a clinician determines the patient’s level based on observation and clinical judgment. It provides a broader picture of the patient’s functional eating abilities rather than specific physiological or anatomical challenges related to swallowing.
Details of the FOIS Levels
- Level 1: Tube dependent with minimal attempts of food or liquid.
- Level 2: Tube dependent with consistent oral intake of food or liquid.
- Level 3: Tube dependent with most nutrition needs met by oral intake.
- Level 4: Total oral diet of a single consistency.
- Level 5: Total oral diet with multiple consistencies, but requiring special preparation or compensations.
- Level 6: Total oral diet with multiple consistencies without special preparation, but with specific food limitations.
- Level 7: Total oral diet with no restrictions.

The Swallowing Quality of Life Questionnaire (SWAL-QOL)
While not a grading scale per se, the SWAL-QOL is a patient-reported outcome measure that assesses the impact of dysphagia on an individual’s quality of life[^3^].
Overview of the SWAL-QOL
The SWAL-QOL is a self-report questionnaire, meaning patients provide responses based on their experiences and perceptions. It comprises various items spread across domains that assess physical symptoms, the psychosocial impact, and the functional consequences of dysphagia.
Domains Covered in the SWAL-QOL
- Symptom Frequency: Evaluates how often the patient experiences swallowing-related symptoms.
- Eating Duration: Assesses the time it takes for patients to finish their meals.
- Eating Desire: Gauges the individual’s appetite and desire to eat.
- Food Selection: Examines any changes or restrictions in food choices due to swallowing difficulties.
- Communication: Determines the impact of dysphagia on verbal communication.
- Fear: Evaluates the level of anxiety or fear associated with eating.
- Mental Health: Assesses the emotional and psychological toll of living with dysphagia.
- Social Functioning: Evaluates the impact of dysphagia on social interactions, especially during mealtimes.
- Fatigue: Gauges the level of tiredness or fatigue associated with eating difficulties.
- Sleep: Determines if swallowing problems interfere with sleep.
The International Dysphagia Diet Standardization Initiative (IDDSI)
The IDDSI framework isn’t a dysphagia grading system, but it does provide standardized terminology for the texture of foods and thickness of liquids for individuals with dysphagia[^4^].
At Refreshment Systems Ltd, we are dedicated to improving the lives of those living with dysphagia. We have collaborated with several manufacturers to develop a unique beverage solution, our dysphagia drinks machine. This innovative solution offers a wide range of beverages adjusted to various IDDSI levels, ensuring that individuals with dysphagia have access to safe and enjoyable drinks.
The Essence of the IDDSI Framework
The IDDSI framework was developed in response to the need for universal terminology for dysphagia diets. Different countries, regions, and institutions often used varied terms to describe similar food textures and liquid consistencies, leading to confusion, inefficiencies, and potential risks.
Components of the IDDSI Framework
- Level 0 – Thin: Regular, unthickened liquids suitable for standard drinking and pouring.
- Level 1 – Slightly Thick: Slightly thickened liquids which are sippable.
- Level 2 – Mildly Thick: Mildly thickened liquids that can be sipped or sucked from a straw and are pourable but flow slower than thin liquids.
- Level 3 – Moderately Thick: Moderately thickened liquids that can be drunk from a cup and can be eaten with a spoon, but may not hold their shape.
- Level 4 – Extremely Thick: Liquids that are usually eaten with a spoon, don’t flow, and hold their shape.
- Level 4 – Pureed: Smooth and cohesive foods that don’t require chewing.
- Level 5 – Minced & Moist: Foods with small, soft lumps that are easily mashed with a fork.
- Level 6 – Soft & Bite-Sized: Foods that are soft, moist, and easily mashed but require some chewing.
- Level 7 – Regular: Normal everyday foods that don’t fit into the other categories.
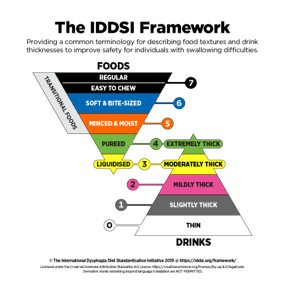
The Value of the IDDSI Framework
- Universal Terminology: IDDSI provides a standardized language that can be understood globally, helping to reduce miscommunication across health care settings.
- Patient Safety: With standardized diet recommendations, the risk of giving a patient inappropriate food textures or liquid consistencies decreases.
- Empowerment and Education: Patients, caregivers, and families can better understand and follow dietary recommendations with clear, standardized guidelines.
- Research and Collaboration: The IDDSI framework provides a common ground for researchers globally, enabling more consistent data collection and collaboration across studies.
Conclusion
Several scales can assess and grade dysphagia, each with its focus and utility. These grading systems, along with innovative solutions like our dysphagia drinks machine, are vital tools in managing dysphagia and enhancing the quality of life for individuals living with this condition.
[^1^]: O’Neil KH, Purdy M, Falk J, Gallo L. The Dysphagia Outcome and Severity Scale. Dysphagia. 1999 Summer;14(3):139-45.
[^2^]: Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005 Aug;86(8):1516-20.
[^3^]: McHorney CA, Robbins J, Lomax K, et al. The SWAL-QOL and SWAL-CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia. 2002 Spring;17(2):97-114.
[^4^]: International Dysphagia Diet Standardisation Initiative, The IDDSI Framework